A study of comparison between premature and full-term babies has revealed immunological differences in cord blood that suggests preterm labor may, at least in some instances, result from fetal intolerance of the mother. The study published in Science Translational Medicine.
Mother-Fetus Intolerance
In pregnancy, both mother and fetus have to be tolerant to each other to have a healthy pregnancy. The fetus's immune system's tolerance to mother is also an important factor - which until now had gone unnoticed. Babies’ immune cells are functional and they would have the potential to reject the mother.
The Study
To examine this hypothesis, researchers at UCSF (The University of California, San Francisco), collected umbilical cord blood from 89 full-term babies and 70 babies whose mothers went into early labor after their waters broke—a condition associated with infection.
The team found major immunological differences between the infants. Cord blood from preterm babies tended to have elevated levels of inflammatory cytokines and activated immune cells, specifically, dendritic cells and memory T cells, compared with that from full-term infants.
Furthermore, preemies had more microchimerism—the presence of maternal cells in their blood—compared with the other babies. And the infants’ T cells were shown to rapidly proliferate in response to maternal antigens. By contrast, T cells from full-term infants did not display such reactivity to antigens from their moms.
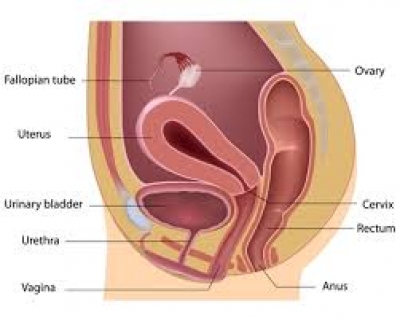
Interestingly, T cells from the mothers of the premature babies were far less reactive to fetal antigens than their babies’ T cells were to maternal antigens, suggesting the intolerance was driven mainly by the immune system of the fetus. The results hinted that T cell activation might promote early birth. But, do these T cells actually contribute to the labor process? The group went on to show that human myometrial cells—the smooth muscle cells of the uterus—contracted more readily when co-cultured with T cells from preterm infants than with immune cells from full-term babies.
What triggers preterm labor?
“Now that they have this association [between intolerance and preterm labor],” says immunologist Mike McCune, also of UCSF but not involved with the work, “the key question is, What initiates it?” The most likely culprit is infection, he says, suggesting that inflammation-driven changes to the placental barrier might increase microchimerism and in turn induce intolerance of maternal antigens. The intolerance would then further amplify the immune response resulting in “an endless and devastating cycle,” he suggests. If such a scenario turns out to be correct, McCune goes on, the next question is, “How can [doctors] detect the process before such time as it causes preterm labor and then prevent preterm labor from occurring?” We will have to find out!